Finding the Path to a Healthier Life
Approaching your 40th birthday, you can’t believe how fast the years have gone by since you graduated from college. It seems like it was yesterday. Then you met your future husband a few years later, got married, eventually working full-time with two children, and constantly stressed from juggling your career and your family. When looking in the mirror trying on a new outfit to wear for your birthday party, you’re frustrated about your weight gain over the years. You were fit and healthy in college when you walked to classes across campus and jogged for an hour every other day. You can’t remember the last time you played tennis with a friend. You used to eat healthier but with your long hours and the children playing soccer or taking music lessons fast-food and Door Dash deliveries have become your go to for dinner meals. As you try on different outfits, you question how did you gain 40# since you were in your twenties?
If you see yourself in this scenario, you are not alone. There are millions of others, both women and men, who are struggling with the same issues. It wasn’t always this way in the US. Until the late 70s, the majority of children were thin, played outside for hours on end, watched television when permitted by their parents, and had their home cooked evening meal around the table with their family. Adults were active, often walking to work or the neighborhood grocery store and rarely ate out. Only one or two children in a classroom and about 1 in 10 adults were obese in 1960-62. Since then, obesity rates in children and adults have tripled.
As a society, how did we get to this point and what are the consequences of the growing obesity epidemic? Is there hope in reversing the trends and if so how do we accomplish that?
The causes of the rapidly increasing levels of obesity are complex and multi-factorial, consisting of metabolic dysfunction and genetic factors interacting with profound environmental and socio-economic changes over the past sixty years. Research indicates that environmental and socio-economic factors contribute the most to the increased prevalence of obesity. A major change over the past century has been a marked decrease in jobs requiring manual labor. In 1909, 38% of Americans worked in farming compared to only 3% in the last decade. Profound nutritional changes and dietary habits such as the consumption of sugar-sweetened beverages and an exponential rise in the number of fast-food restaurants and eating out have fundamentally altered the American diet.
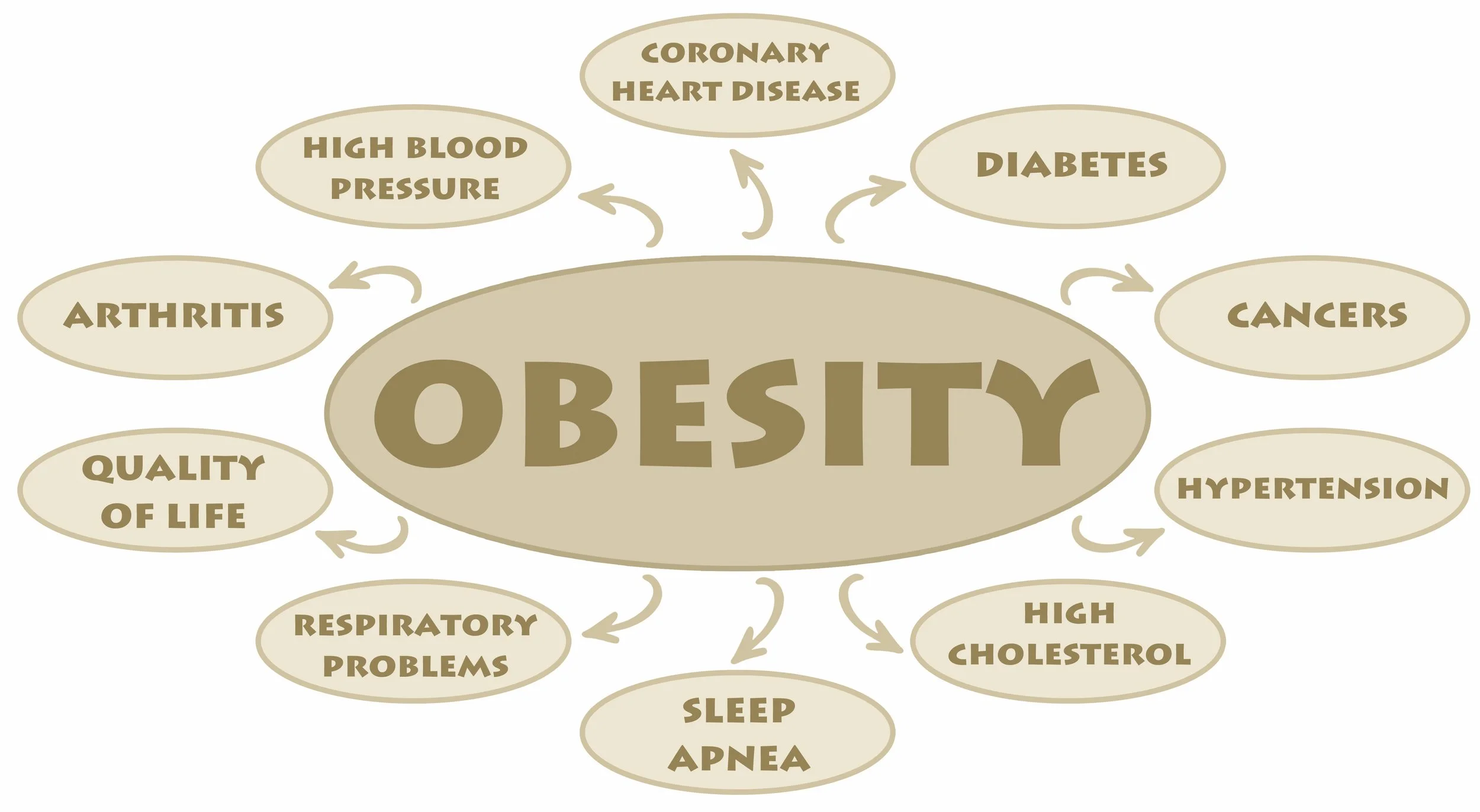
How much you weigh is very important to your health as obesity contributes to Type II diabetes, cardiovascular disease, obesity-related cancers, and increased risk of premature death. Fat is not just a storage for excess calories but is in fact active in producing and releasing a number of hormones and proteins into the circulation. Studies show that a weight gain of just 7-10# can contribute to insulin resistance, making further weight gain easier and increasing the risk of developing Type II diabetes. Carrying an extra 40-60# is a major cause of degenerative joint disease (DJD), specifically on knees and hips, the two major weight-bearing joints. Nearly 1.5 million knee and hip replacement surgeries were done in 2020, with projections that these two procedures will likely double over the upcoming decade as a result of the obesity epidemic.
Being overweight or obese carries with it a higher cost of healthcare, especially when it leads to Type II diabetes where over $300 billion is spent each year on direct medical costs, lost wages, and productivity.
What is the Body Mass Index (BMI) and how is it used?
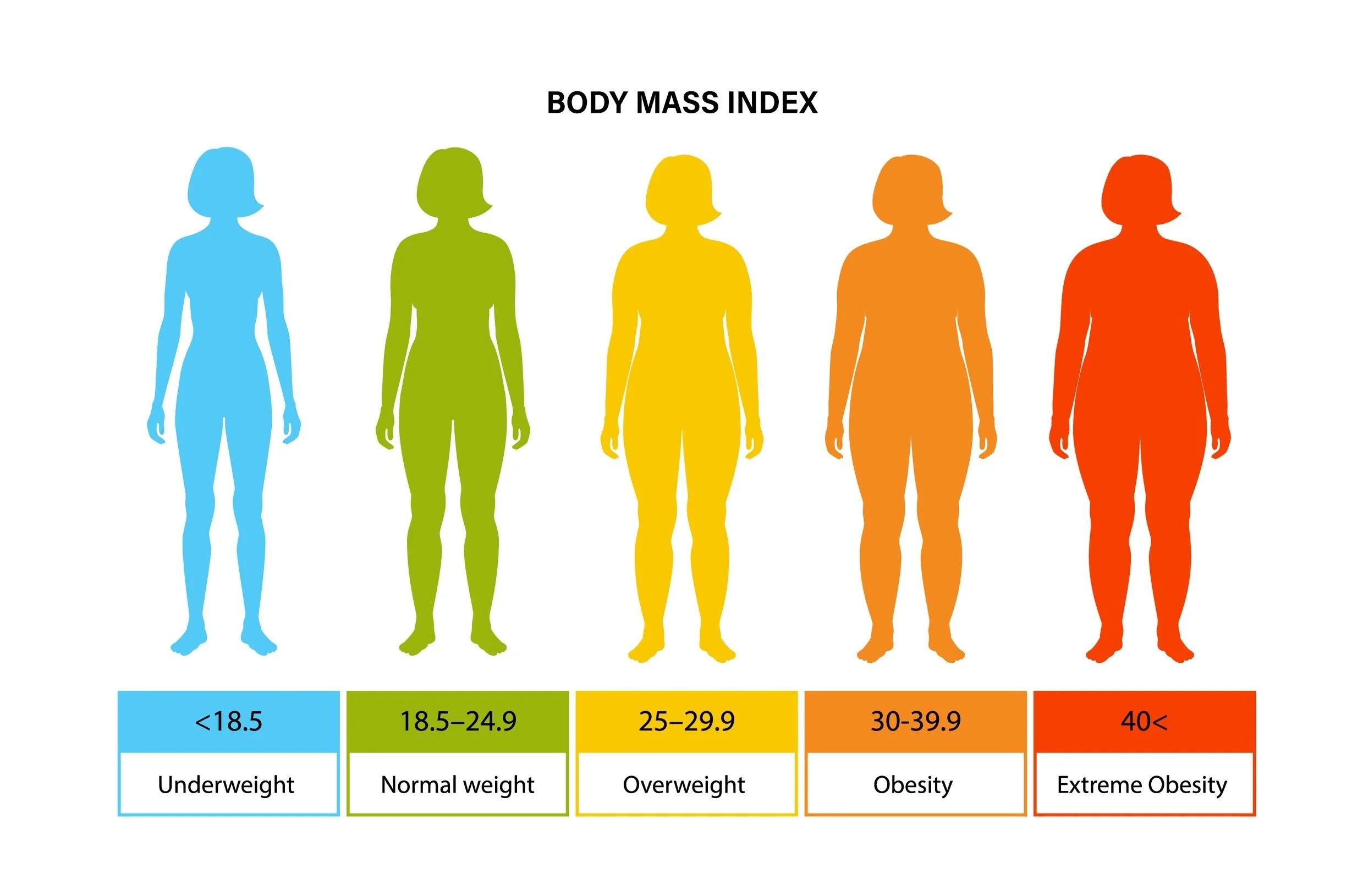
Being overweight or obese represents health conditions in which an individual’s weight is higher in relationship to their height. Body Mass Index (BMI) is the standard measurement tool used for categorizing levels of underweight, normal, overweight, obesity, and severe obesity across the world. It is calculated by dividing the person’s weight measured in kilograms by height in meters squared. Since children are growing taller and gaining weight, childhood levels of overweight or obese are based on percentiles of BMI scoring. Since BMI does not distinguish fat from muscle or bone, it is less useful in athletes and heavily muscled individuals. For these individuals, calculating total body fat utilizing several available measurement methods will be more useful.
The BMI is used to place individuals in risk categories, based on long-term research linking elevated levels of body fat to an individual’s risk of death, developing Type II diabetes, cancer, cardiovascular disease, and other chronic medical conditions. During the recent COVID-19 pandemic, a high BMI was shown early on to be a strong predictor of a more prolonged and serious illness and death.
The illustration below portrays a person’s body shape according to their BMI.
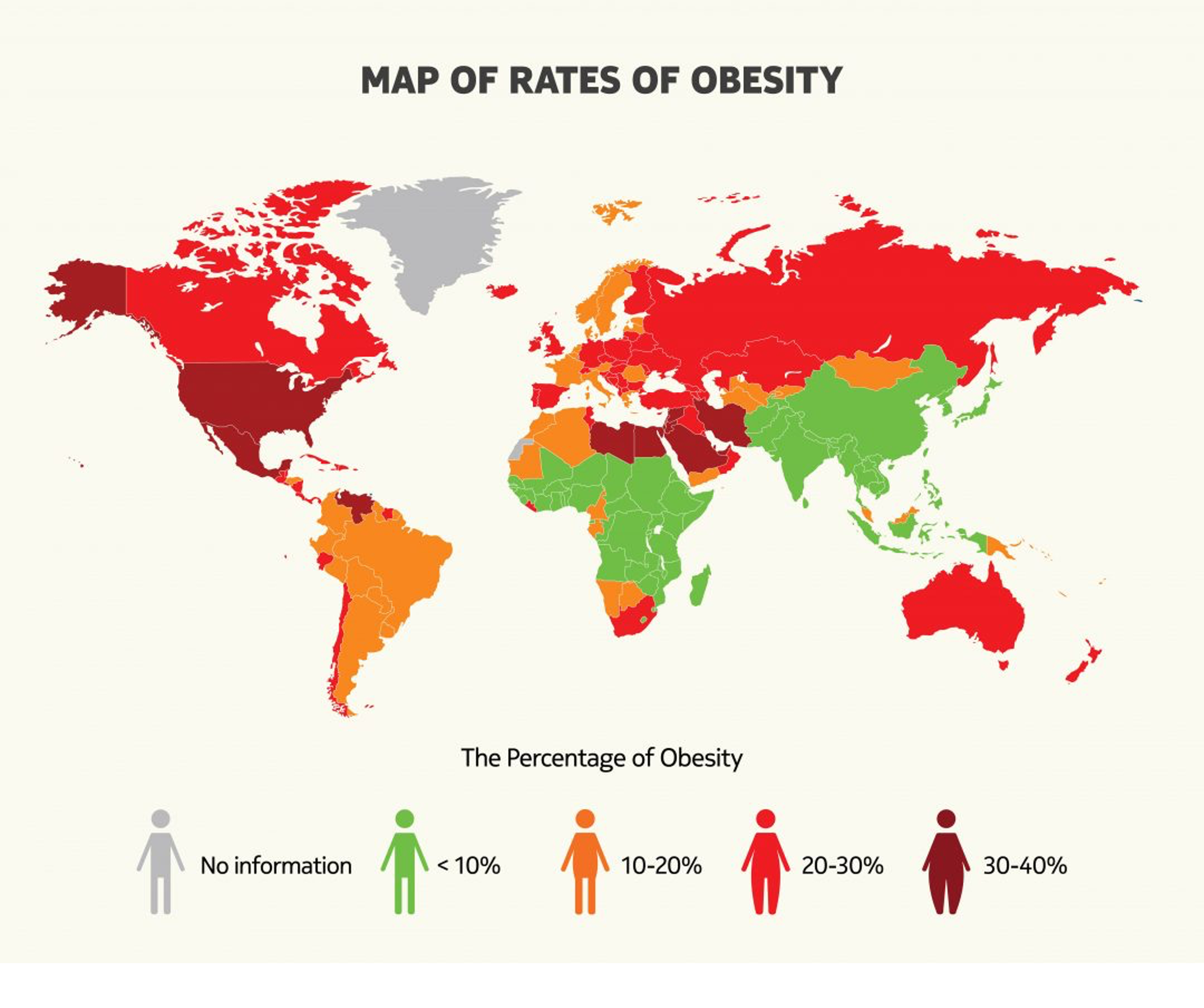
State Surveys
Based on a self-reporting survey in 2022, all states have obesity rates above 25%. As of 2023, the states with obesity rates above 40% are West Virginia, Mississippi, Arkansas, and Louisiana. Tennessee, Alabama, Ohio, Wisconsin, and Kentucky rank close behind. High obesity rates correlated with lower average annual income and high rates of poverty. In comparison, the District of Columbia, Hawaii, Colorado, Massachusetts, and California are the states with the lowest obesity rates, all sitting around 25%. Low obesity rates correlate with higher average annual income and lower levels of poverty.
Effects on health and complications from excessive weight
Carrying excess weight has direct links to many chronic health conditions affecting millions of people world-wide with Type II diabetes being the most well-known association. Diabetes is the leading cause of chronic renal failure requiring dialysis, blindness, and causes 80% of all amputations of the toe, foot, or legs in the US.
Most people are unaware of the relationship of excessive weight to the higher risk of developing 13 different types of cancer. Furthermore, these 13 types of cancer make up 40% of all types of cancer diagnosed in the US with all obesity related cancers totaling over 680,000 people.
Multiple mechanisms have been proposed to explain why excess fat tissue contributes to higher risks of cancer. The increased risk of cancer may be related to the high amounts of estrogen produced by fat cells (especially in post-menopausal women), higher levels of insulin as well as production and release of proteins that enhance cancer cells to grow and spread.
Why are we in this pandemic?
https://www.scientia.global/wp-content/uploads/Jamie_Baum/fg_2-1080x864.jpg
How did we get here in just sixty years? Obesity was rarely seen in the past 25,000 years of human existence as our ancestors moved from the Stone age to the Middle Ages and the 17th century. Analysis and reconstruction of our ancestors’ bodies suggest that the body fat composition (what percentage of the person’s weight is coming from fat stores)in men was only 2-3% and was under 10% in females in comparison to current levels of 40% in women and 28% in male.
Obesity has increased to pandemic levels in populations where environmental changes have led to physical inactivity along with increased consumption of high-calorie foods and larger meal portions. Yet, there are individuals who are inactive and consume high-calorie foods who do not become obese. This paradox suggests that one’s genetic make-up does play a role in obesity.
Research indicates that obesity is not simply a personal choice of overeating or being lazy, a stigma that is still widely prevalent. To effectively treat this disease or prevent it from developing in the first place, medical professionals are encouraged to abandon a judgmental perspective and to accept the position that obesity is a disease, a consensus statement from the June 2013 American Medical Association (AMA) annual meeting with additional support from national endocrine societies, The American College of Cardiology, the American Heart Association, and others. Although the NIH declared obesity as a disease earlier in 1998 and the American Obesity Society did likewise in 2002 these organizations do not carry the same reputation and influence as the AMA for policy setting, research initiatives, and prevention.
The increase in obesity rates over the past fifty years has not arisen from dramatic changes in human metabolism or genetic factors. Rather, society has markedly changed in many areas. Fewer people have jobs in farming, auto industry, steel industry and other manual labor jobs, replaced by service jobs with less activity and lower pay. Changes in the types of food we eat, where we eat, and how much we eat play a major role in the obesity epidemic. Leisure time for both adults and children has been transformed by the increase in time spent on smart phones, listening to music, watching television, and playing video games.
What is insulin resistance and how does it affect weight gain?
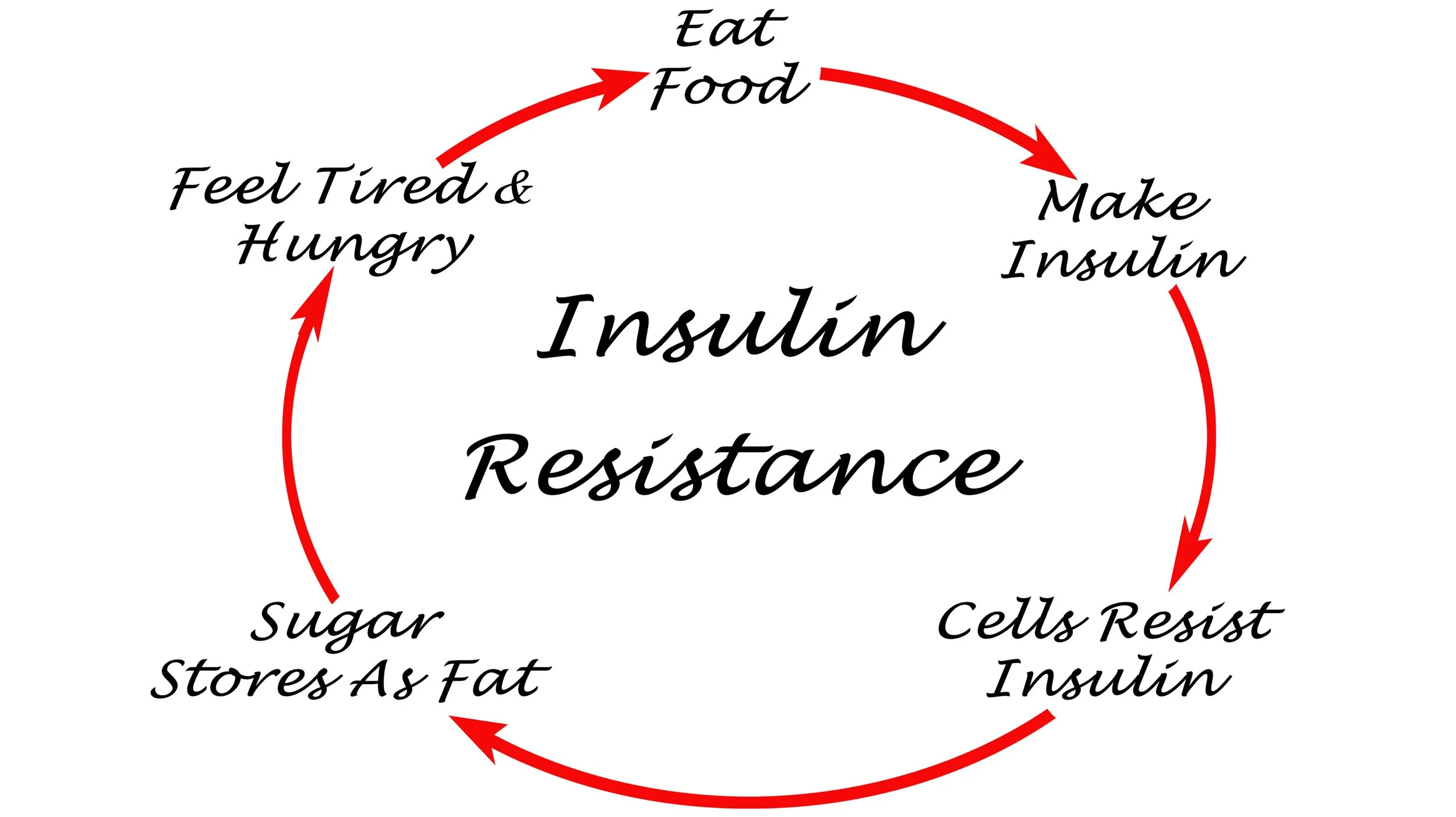
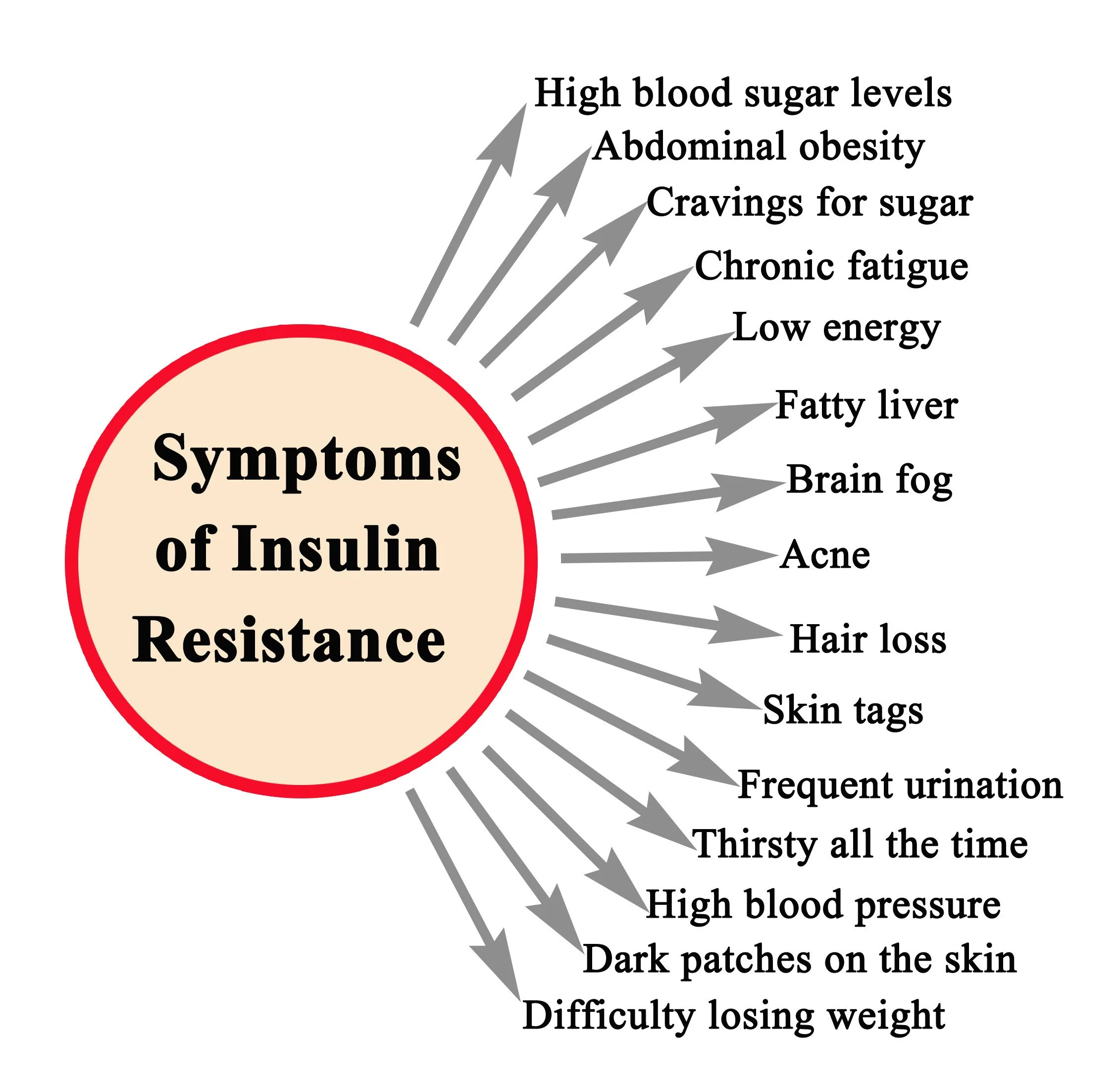
One of the most common hormonal dysfunctions that contributes to weight gain is insulin resistance, and if untreated leads to Type II diabetes. The American Diabetes Association states that people with insulin resistance have built up a tolerance to insulin, the hormone responsible for flipping blood sugars into the body’s cells for generating energy, making the hormone less effective Thus, the vicious cycle is depicted below.
As mentioned previously, it can take only a minimal amount of weight gain, as little as 7-10# to tip the balance towards insulin resistance. The following diagram depicts the various symptoms of the disorder, often beginning with fatigue and being hungry all the time.
Weight gain over the holidays or from a weeklong cruise may be the trigger for some people. An injury that affects the individual’s routine of work and play and makes them less active contributes to insulin resistance. Excessive weight gain during pregnancy contributing to pre-diabetes or gestational diabetes is a common factor. An alarming fact is that up to 70% of mothers with gestational diabetes develop Type II diabetes within 20 years.
Increasing waist size is an indicator that the body is storing excessive blood sugar inside of the abdominal cavity, referred to as visceral fat. Medications can have a profound effect on weight gain and insulin resistance. A five-day course of oral steroids for a case of bronchitis or an allergic rash may cause more dysfunction in this system. In addition, some medications used to treat patients with depression or bi-polar disorder are noted to cause weight gain, which may then trigger insulin resistance. Metformin, a medicine used to lower blood sugar, also lowers insulin resistance, and has been used as add-on therapy to antidepressants to treat insulin resistance. In addition, studies suggest that metformin itself may have a positive effect on depression.
Can I be evaluated for insulin resistance?
Yes! The HbA1c blood test can be used as a diagnostic tool for the early detection of insulin resistance. The test measures what percentage of the red blood cells have a sugar molecule attached to them. A value under 5.7% is considered normal, between 5.7% and 6.4% is considered prediabetes and a value at or above 6.5% is diagnostic for diabetes.
Genetic factors
Despite the common perception that genetic predisposition is the main cause of their obesity, “Obesity runs in my family”, only a handful of the 400 different genes identified as potentially affecting weight gain have a dominant role in the development of obesity. Studying similarities and differences among family members, twins, twins separated at birth, and adopted children led to the conclusion that a proportion of the variation of obesity in adults comes from genetic factors. No single gene leads to a clear and consistent path to obesity.
Genetic testing for obesity is still at the research level. Although there are companies promoting commercial tests claiming accurate assessments of genetic predisposition to obesity, more scientific studies need to be done to confirm their usefulness for widespread clinical use. So, “let the buyer beware.”
An obese individual is more likely to carry a significant genetic component if it runs in the family, the person has been overweight or obese most of their life, has a BMI over 35 and is unable to lose weight when physically active and following a healthy diet. In comparison, an overweight or obese individual who is successful in lowering their BMI with diet and exercise but regains weight and goes through several weight loss/weight gain cycles is less likely to carry genes responsible for weight gain
Summary
It is clear that the levels of being overweight or obesity based on BMI scores have increased dramatically in children, adolescents, and adults over the past fifty years. Levels of obesity across the country are clearly linked to income, with the highest levels correlating to states with lower annual incomes. The cause of the dramatic increases in weight are complex and multi-factorial. Genetics do play a role in some people but the overwhelming consensus is that lifestyles and socio-economic factors play the biggest role.
So, when you are standing in front of that mirror, acknowledge your family history of Type II diabetes on your mother’s side and realize you likely have insulin resistance, triggered by the 25# you gained from the first pregnancy and then worsened by the 30# weight gain from your second pregnancy. You then found yourself in this vicious cycle depicted in the illustration above. But be hopeful. With lifestyle changes and sometimes the use of certain medicines to treat insulin resistance, you can restore the normal balance in your body.
In the next segment, these environmental and society changes will be explored in more detail.